
To learn more about our RealSuture 6-Layer Suture Pad click here.
If you're planning to practice suture techniques, your choice of training materials makes a big difference. Pigs’ feet and banana peels may work in a pinch, but suture training pads are vastly superior in every respect. However, as with all things, not all suture pads are created equal.
Getting a clear sense of the skills you want to practice will help ensure you select the right suture pad for your needs. For students just starting out, beginning with a simple pad will help to fine-tune basic techniques. In contrast, if you want to practice more advanced techniques, such as buried and subcuticular sutures, you’ll need a more complex pad to use for practice.
If you’re wondering which suture pad is right for you, here are some key factors to consider.
Begin With Visibility: The Translucent Pad
For students just getting started on suture techniques, a translucent pad may be a good place to start. The translucence allows you to more accurately see sutures under the skin, gauge the depth and spacing, and generally get a clear sense of what you are doing with each stitch.
A translucent suture pad allows for a 3D understanding of your work, and is sufficient for everything a beginning student needs to practice. These pads allow you to practice superficial sutures (simple interrupted, simple continuous, interrupted), knot security, and basic patterns.
This pad also comes with optional pre-cut incision and suture guide dots to remove any guess work for beginners. Guide dots are important because the insertion point of your needle needs to be equal distance from the incision, the point of insertion above it, and the point of insertion below it. Any inconsistency, and you will have uneven pulling and a higher chance of scarring.
Practice Realism: The 3-Layer Pad
Once you’ve mastered the basic techniques on a translucent pad, moving on to a 3-layer pad will provide a more realistic experience since it closely resembles human tissue. This pad mimics the first three superficial layers of the abdominal wall — dermis/epidermis, subcutaneous fat layer, and fascia. To behave like real tissue, the epidermis layer has been reinforced to absorb tension and pulling in your suture practice. As with the single-layer pads, the 3-layer pads are ideal for superficial sutures and ensuring knot security.
Importantly, these pads (as well as the 5-layer and 6-layer pads) come in dark skin tones as well as light. Practicing only on light skin training pads will not adequately prepare students for the diversity of skin tones they will encounter in real world settings. Suturing on darker skin is more difficult — as suture visibility is more challenging when the contrast between skin and monofilament is lower. Failing to practice on a range of skin tones can lead to poor suturing, which results in higher incidences of scarring, increased rates of infection, and longer healing times for patients.
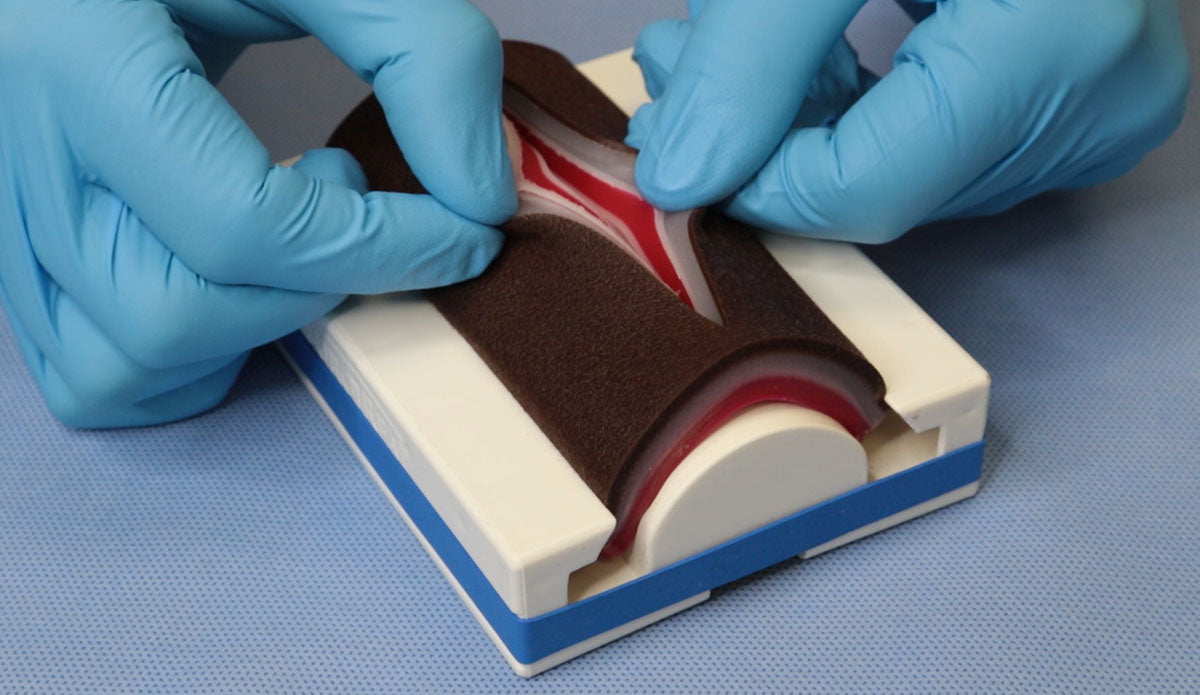
Advanced Techniques: The 5-Layer and 6-Layer Pads

For students already comfortable with the basic suturing techniques, the more complex suture pads provide opportunities to practice advanced techniques. In addition to everything offered in the 3-layer pad, the 5-layer pad allows for a second layer of closure and buried sutures. The layers replicate the epidermis, subcutaneous, first fascia layer, muscle, and second fascia layer.
Buried sutures distribute wound tension to the dermis and thereby improve cosmetic results in the healing tissue. Since the suturing occurs at the subcutaneous level, it’s important for the suture pad to be equipped with sufficient layers to support the technique.
If you want to practice subcuticular sutures, you will need a 6-layer pad. This high-quality product will do everything that the 3-layer and 5-layer pads will do, with the added option of allowing you to practice the most advanced techniques. The 6th layer comes from a separated and reinforced dermis and epidermis layer, which makes it the only sufficiently reinforced pad for practicing subcuticular sutures.
Again, both our 5-layer and 6-layer pads come in both light and dark skin tones. Our goal has always been to improve student confidence, and providing students the opportunity to practice on a range of skin tones is one way to help the industry improve outcomes for all individuals.
Dermal Lesions and Other Specialty Techniques
In addition to the features necessary for standard suture practice, our 5-layer and 6-layer pads both include simulated moles to provide an opportunity for practicing mole biopsy and mole removal. For more in-depth practice in mole and lesion removal, we created a 3-layer dermal lesion pad. In addition to mole removal and skin reconstruction, this specialty pad provides students with the opportunity to practice various biopsy methods including: punch, shave, excisional, and snip biopsy. We also offer training pad options for practicing incision and drainage, as well as injections.
A Commitment to Comprehensive Training
Regardless of starting point — from absolute beginners to seasoned practitioners looking to refresh skills — SurgiReal has created the most realistic and affordable training models available. Our suture training pads were designed to give practicing students the most realistic tissue feel without the need for cadavers. By continuing our commitment to accuracy and affordability we hope to encourage students and practitioners to seek out the best tools in their practice and studies.
If you still have questions about which suture pad might best fit your needs, please don’t hesitate to reach out.
To learn more about our RealSuture 6-Layer Suture Pad click here.
